As you help MassHealth members with their renewals over the next several months, you may find that some people may no longer be eligible for MassHealth coverage.
Instead, people may newly qualify for a subsidized Health Connector plan, with Advanced Premium Tax Credits (APTCs) or a ConnectorCare plan. Others may not qualify for any subsidy – or help paying for their premium, but they may be able to enroll into an unsubsidized Qualified Health Plan (QHP) through the Health Connector. While others may not be eligible for health coverage through the state.
MassHealth coverage will end for those newly qualifying for Health Connector coverage on two different timelines. Here is a reminder of the policy that MassHealth and the Health Connector have in place.
- For anyone that becomes ineligible for MassHealth, moving to an unsubsidized QHP or not eligible for any other coverage, they will lose their MassHealth benefit 14 days after the date of their eligibility termination notice.
- For anyone moving to a subsidized QHP (ConnectorCare or APTC only):
- If the MassHealth coverage end date occurs on or before the 15th of the month they will maintain MassHealth benefits until the end of the month. For MassHealth coverage to end on the 15th of the month, the termination notice would need to occur on the first day of that month. If the termination notice occurs after the first day of the month, MassHealth coverage would end after the 15th and coverage would be extended until the month following.
- If the MassHealth coverage end date occurs after the 15th of the month, they will maintain their MassHealth benefit until the end of the next (following) month.
Sample Member Scenario
As an example, if Louisa completes her renewal on May 4th and finds out that she is no longer eligible for MassHealth but is newly eligible for an unsubsidized plan (a QHP) through the Health Connector, her MassHealth coverage will end on May 18th.
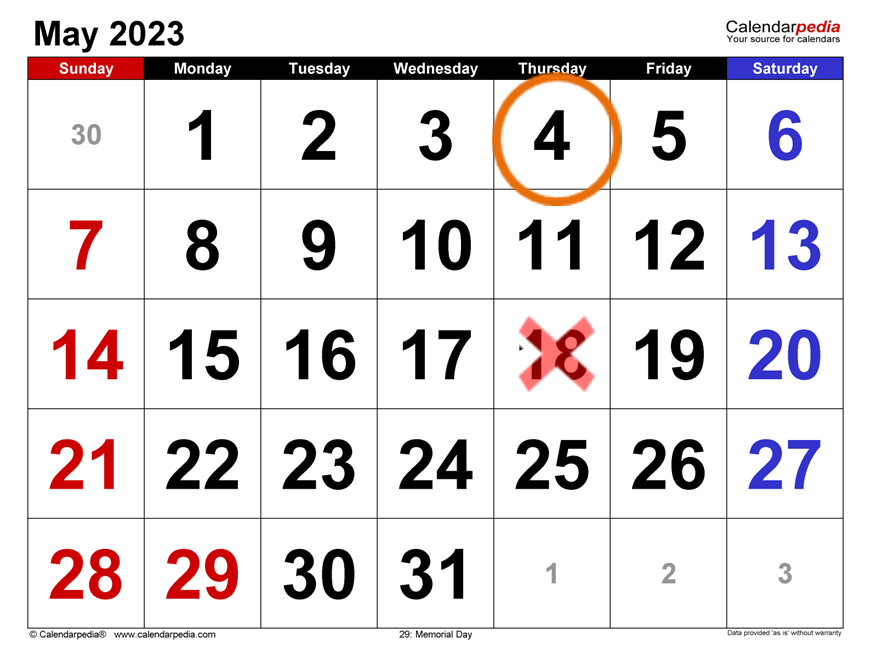
However, if Louisa completed her renewal on May 4th and found out that she is no longer eligible for MassHealth but is newly eligible for ConnectorCare or a QHP with APTCs, Louisa would maintain her MassHealth coverage until the end of June.
Enrolling in ConnectorCare Coverage
Louisa has the option to enroll in ConnectorCare coverage that begins on June 1, as long as she selects a plan, pays the premium (if one is owed) and enrolls by May 23rd.
To avoid a gap in coverage, Louisa must select and enroll in ConnectorCare by June 23rd for a plan that would be effective for July 1.

If Louisa does not take action by 6/23, she would still have an extended Special Enrollment Period (SEP) through the Health Connector until November 23, 2023, but she would also have a gap in coverage until she does enroll.
Note: In this scenario, there could be many months that Louisa does not have health insurance coverage. Remember, although the SEP runs through 11/23/23, she has the option to enroll in coverage before that deadline.

The complete policy can be found here: MassHealth regulation: 130 CMR 502.006(D): https://www.mass.gov/doc/130-cmr-502000-masshealth-the-eligibility-process-0/download.



